Life care planners frequently create life care plans for people with chronic pain due to injury and disability. The federal government estimates more than 50 million adults live with chronic pain costing the country $560 billion annually in medical care, disability benefits, and lost productivity.[1] Chronic pain can affect a person’s family and social relationships and ability to work,[2] and lead to depression and hopelessness. Chronic pain can affect any body part, with the lower back and headaches being the most frequent.
In personal injury cases, chronic pain can significantly increase future costs of treatment, future loss of earnings and future loss of household services. Life care planners, working with consulting and treating physicians, play a valuable role by creating a long-term plan that increases a person’s quality of life, decreases the need for costly and invasive future procedures, and returns them to their careers and family responsibilities.
Chronic pain is difficult to treat in part because chronic pain may continue after the original source of the pain has been treated and healed. Long-term pain can cause permanent changes to the nervous system that change how a person perceives pain. The person perceives severe pain with little to no pain stimulus.[3] People with chronic pain may become less active and less independent fearing worsening the pain or further injury. Depression can be a common co-morbidity with chronic pain, affecting 30-80 percent of this population, making the pain sensation more intense and difficult to treat.
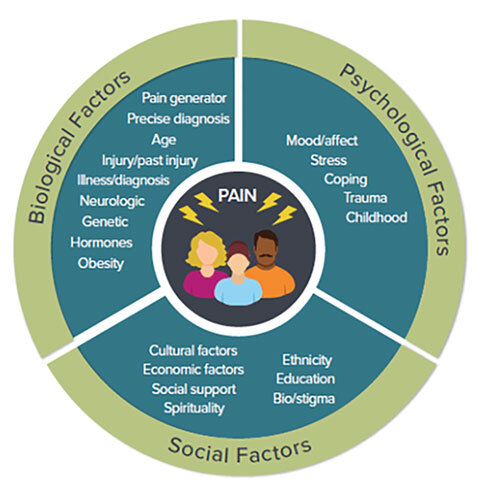
Recent practice guidelines developed by the Veterans’ Administration and the Department of Defense and endorsed by the DHHS Pain Management Best practices Inter-Agency Task Force, recommend clinicians use a biosocial model of pain as illustrated in the diagram below[4].
The DHHS Interagency Task Force on Pain Management Best Practices identified five treatment approaches:
- Medication
- Restorative Therapies
- Interventional Procedures
- Behavioral Health Approaches
- Complimentary and Integrative Health
There appears to be a consensus that too much reliance has been placed on injections, surgery, and opioid medications. The benefits of opioid medications decline with long term use due to physiologic tolerance. In 2016, the Centers for Disease Control and Prevention recommended against opioids as first-line treatment of chronic pain. And doctors have become more cautious, leading to a decline in prescribing rates. The effects of medications limit the activities a person can safely perform. A concern for addiction and misuse[5] is causing government and clinicians to revise treatment guidelines and redefine best practices. A life care planner should be current with these developments.
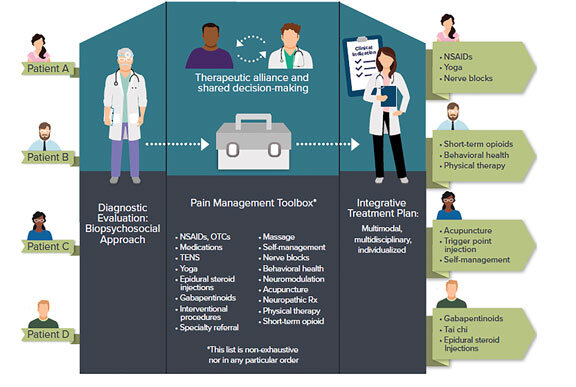
Best practices call for individualized patient care based on a diagnostic evaluation that results in an integrative treatment plan that includes all necessary treatment options as shown in the diagram below.[6]
When assessing the future care needs of a person with chronic pain, the life care planner, in collaboration with treating or consulting physicians, should critically analyze whether to recommend continuing the current treatment or recommend alternative approaches to management of chronic pain.
- According to the National Institutes of Health, a growing body of evidence suggests approaches such as acupuncture, hypnosis, mindfulness meditation, spinal manipulation and yoga may help to manage chronic pain. Research also supports cognitive behavioral therapy, which teaches patients skills to overcome negative thoughts and behaviors, as a cost-effective way to manage some chronic pain.[7]
- Interdisciplinary pain rehabilitation programs are available in most major metropolitan areas. The goal of these programs is to reduce a person’s dependence on opioid pain medications and facilitate them returning to work and social activities. The programs usually last three to six weeks and employ multiple treatment modalities, including medical management, physical and occupational therapy, pain psychology, relaxation therapy, counseling, vocational rehabilitation services, nursing education, and aerobic conditioning.[8]
- Non-pharmacologic and non-opioid pain management plans may reduce or end reliance on opioid medications. These include many of the same elements as the structured pain program but rely on non-opioid pharmacologic interventions such as non-steroidal anti-inflammatory drugs (NSAIDS), acetaminophen (Tylenol), or corticosteroids when appropriate. [9]
The life care planner should take a holistic view of the person with chronic pain in their biosocial setting and design a care plan that considers all five approaches to maximize the person’s ability to manage pain in ways that also maximize quality of life, productivity, and independence.
____________________________________________________________________________________________________________________________________
[1] Dahlhamer J, Lucas J, Zelaya, C, et al. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults — United States, 2016. MMWR Morb Mortal Wkly Rep 2018;67:1001–1006. DOI: http://dx.doi.org/10.15585/mmwr.mm6736a2external icon.
[2] American Chiropractic Association. Chronic Pain and Depression. www.acatoday.org. Accessed May 19, 2019.
[3] American Society of Regional Anesthesia and Pain Medicine. Types of Chronic Pain. www.asra.com. Accessed May 19, 2019.
[4] U.S. Department of Health and Human Services (2019, May). Pain Management Best Practices Inter-Agency Task Force Report: Updates, Gaps, Inconsistencies, and Recommendations. Retrieved from U. S. Department of Health and Human Services website: https://www.hhs.gov/ash/advisory-committees/pain/reports/index.html, p.19
[5] AMA Journal of Ethics. Long-Term Opioid Treatment. www.journalofethics.ama-assn.org. Accessed May 22, 2019.
[6] DHHS, op. cit., page 21.
[7] Laura Landros, “A New Prognosis for Pain Care,” Wall Street Journal, February 6, 2019
[8] Santos, Steven. “Focused Review of Interdisciplinary Pain Rehabilitation Programs for Chronic Pain Management.” Current Pain and Headache Reports. 2012 Apr;16(2):147-52.
[9] The Joint Commission. Non-pharmacologic and non-opioid solutions for pain management. www.jointcommision.org. Accessed May 22, 2019.
