Author
Author: Rachel Short, MPH
Certificate of Need (CON) requirements vary by state, but many require applications to address three main topics: need, financial feasibility, and impact on existing providers. This is the third and final part of this three-topic series. This blog post discusses data sources to address the impact on existing providers of a CON-reviewable project.
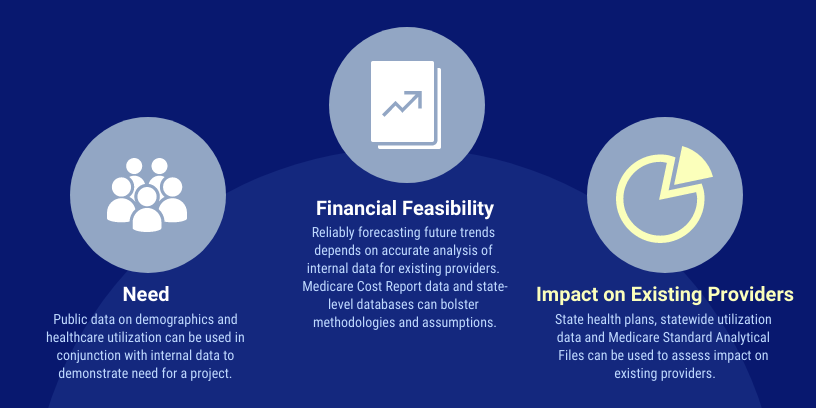
A cornerstone of CON programs is controlling health care costs by avoiding duplication of services. Because of this, many states require applicants to show that a proposed project will not materially negatively affect existing providers. Most states allow existing providers to appeal the approval of a new provider, and argue the new entrant would adversely impact their operations and finances. Therefore, applicants must show there will be sufficient demand that their project will not greatly reduce the volume at existing providers below their volumes in the baseline year. A number or public and private data sources can help an applicant show this. Below we will explain those sources and show example of their use.
Public Data Sources
Federal Data
The Center for Medicare and Medicaid Services (“CMS”) collects financial and utilization data for many types of healthcare providers including hospitals, ambulatory surgery centers, hospices, nursing homes and home health agencies. Medicare Standard Analytical Files (“SAF”) contain all fee-for-service Medicare claims for services rendered during a calendar year. For certain services where Medicare is the largest payor (e.g. hospices and inpatient rehabilitation hospitals), SAF data provides a valuable tool for assessing market shares of existing providers. SAF data can allow a market entrant, or the opponents, to determine how the proposed project will impact patient volume and Medicare revenue. SAF data permits detailed analysis based on patient diagnosis, procedure codes, and place of service. SAF data for several recent years can show trends.
For an existing provider proposing to enter a new market, SAF data can show whether the provider has had an adverse impact on existing providers in another market it entered. SAF data can quantify utilization (admissions, patient days, procedures, etc.) before and after a provider enters a market. This will show if existing providers in a market saw volumes decline.
Medicare Cost Reports (“MCRs”) are a subset of the cost report data in the Healthcare Provider Cost Reporting Information System (HCRIS) that CMS makes available for public use. MCRs provide useful information for assessing potential financial impact on existing providers. MCR data show a provider’s financial health over time using metrics such as net patient income, operating margin and additional income sources, like foundation contributions and grants. MCRs also have data on volume and payor mix. They can be the basis for arguments about a provider’s financial vulnerability to new market entrants.
IRS Form 990s have data on executive compensation of private tax-exempt providers, such as hospitals, hospices, and nursing homes. This information can be very useful if a nonprofit entity claims financial harm or vulnerability but gives large compensation package to its executives. Form 990s can also provide detail on financial support healthcare providers receive from related foundations.
State Data
Data available varies significantly from state to state. However, many CON states publish need publications or state health plans. These documents contain utilization data which can be used to compare volume trends for a particular provider, service, or geographic market. These data also allow potential CON applicants to compare geographic areas to identify those where existing providers did not serve as many patients as expected for a market of similar size. Such information may allow an applicant to argue that its entrance into a market will increase utilization of services to a better level for residents.
CON decisions and findings, often published online, provide useful, detail on any approved but not yet operational providers. In many states, approved providers are counted against the inventory of needed services. Even for states or services where there is no numeric need determination, an approved provider may argue the state should not approve another provider before giving it time to fully ramp up services.
Previous CON Applications often include detailed information on an established provider’s historical and projected utilization, payor mix, gross and net patient revenues. A provider may assert its financial health a CON application to prove its financial feasibility. When preparing a CON application, an applicant should review applications recently filed by existing providers to gain insight into service line planning, physician recruiting, and charity care policies. Representation in past applications may prevent an existing provider from making an adverse impact argument.
RPC Data Resources
RPC has experience using all the data sources discussed in this post when assisting our client on CON matters. We have Data Use Agreements for all CMS Standard Analytical Files. We have used many state data files. We have the IT resources and staff expertise to analyze large internal data bases from physician practices, hospitals, and other facilities. By combining data expertise with health planning expertise and experience, we can effectively address the impact on existing providers in the CON process.

